
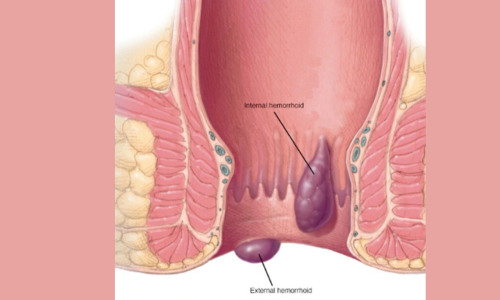
Important Disclaimer: “Piles” is the common term for hemorrhoids—swollen veins in the anus/rectum causing bleeding, pain, itching, or prolapse. Surgery is rarely needed (only ~5-10% of cases). Most resolve with diet (high fiber, 30-35g/day), hydration, stool softeners, topical creams, or office procedures (rubber band ligation, sclerotherapy, infrared coagulation). Surgery is for Grade III-IV (prolapsing, not reducing manually) or failures of non-surgical treatments. This is general info—consult a colorectal surgeon/proctologist for personalized advice. Sources: ASCRS guidelines, recent meta-analyses (2023-2025).
Hemorrhoids graded I-IV (Goligher classification):
Aaradhya Nursing Home provides reliable and compassionate medical care for diabetes, hypertension, thyroid, and general health issues. Led by Dr. Ankita Singh (MBBS, MD), we are committed to delivering accurate diagnosis and patient-focused treatment.
Aaradhya Nursing Home provides reliable and compassionate medical care for diabetes, hypertension, thyroid, and general health issues. Led by Dr. Ankita Singh (MBBS, MD), we are committed to delivering accurate diagnosis and patient-focused treatment.
Aaradhya Nursing Home provides reliable and compassionate medical care for diabetes, hypertension, thyroid, and general health issues. Led by Dr. Ankita Singh (MBBS, MD), we are committed to delivering accurate diagnosis and patient-focused treatment.
© 2025 Aaradhya Nursing Home Powered by GL Service & Solutions Pvt Ltd